Affecting over 300 million people worldwide,
ASCVD is a disease that threatens
all nations and races1.
80% of premature cardiovascular events can be prevented2. By exposing the realities
of ASCVD, we can change the course of this disease and the fate of an Invisible Nation.
Educating people about the risk factors and consequences of
ASCVD will help achieve better outcomes
Who is at Risk?
Given how widespread and devastating this chronic disease can be, it is important to identify who is vulnerable1,3-5. Key causes of ASCVD include high levels of cholesterol (dyslipidemia), high blood pressure (hypertension), smoking, diabetes, family history and certain genetic pre-conditions, such as inherited high cholesterol that starts at a young age (familial hypercholesterolemia or FH). Other risk factors that contribute to ASCVD include a poor diet, low levels of physical activity, being overweight, excessive alcohol intake, and stress. Age and gender are also contributory factors, especially in women after menopause.

Gender

Smoking

Overweight

High Blood Pressure
Diabetes mellitus

Lack of Exercise

Close relatives with heart attack in men under 55 and women under 65 years of age
Age
Steps we can take
Some of the causes that lead to ASCVD are outside of our control. However, there are several risk factors that we can take control of. By focusing on these, we can significantly reduce the risk of developing ASCVD.
Physical Activity
Aim to move more and reduce your sitting time. Small changes such as taking the stairs instead of the lift can make a big difference to your health. Being active is a great way to strengthen your heart muscle, manage your cholesterol, weight and blood pressure and most importantly makes you feel good.
Heart-healthy diet
Limiting our intake of saturated fat, alcohol, sugar and salt can help reduce our cholesterol, blood pressure, weight and risk of diabetes.

Managing Stress
Being stressed or anxious may bring on symptoms like angina or chest pain but developing ways to cope with stress can reduce its effect on your health.

Quitting smoking
Smoking doubles your risk of developing heart disease. If you are a smoker, the single most important thing you can do is to stop smoking!
Regular check-ups
Visit your doctor and get your blood pressure and cholesterol levels checked. Everyone should have their first cholesterol screening test by age 35 for men, and age 45 for women6. Blood pressure should be checked every 2 years7. Those who are at higher risk should consider more frequent assessment: those taking medicines to lower cholesterol levels should be offered a cholesterol test every year8.
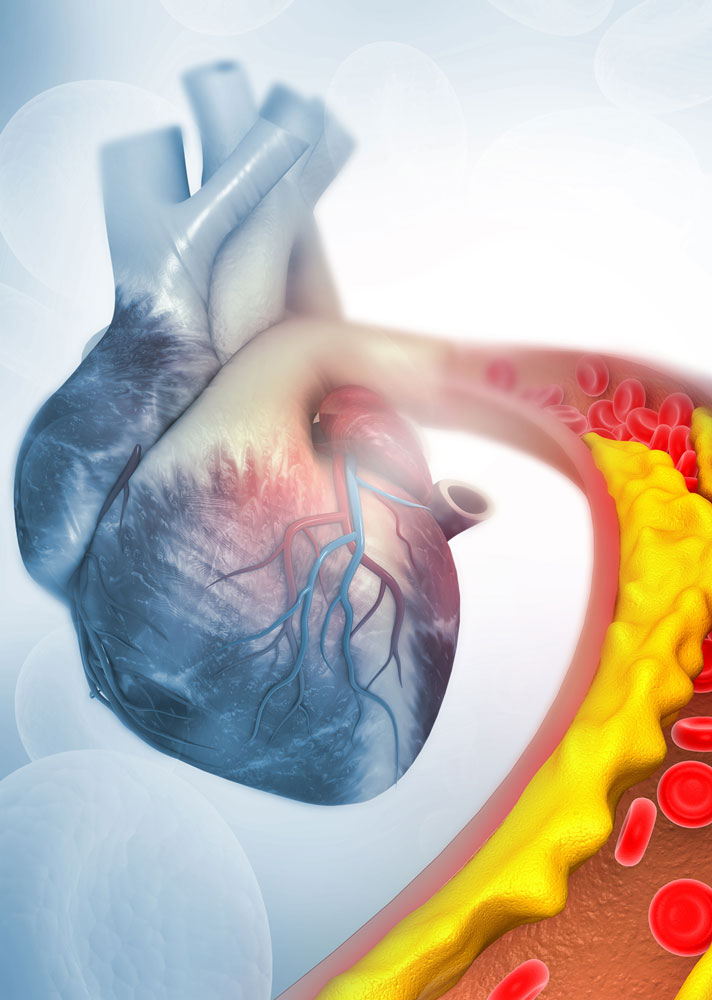
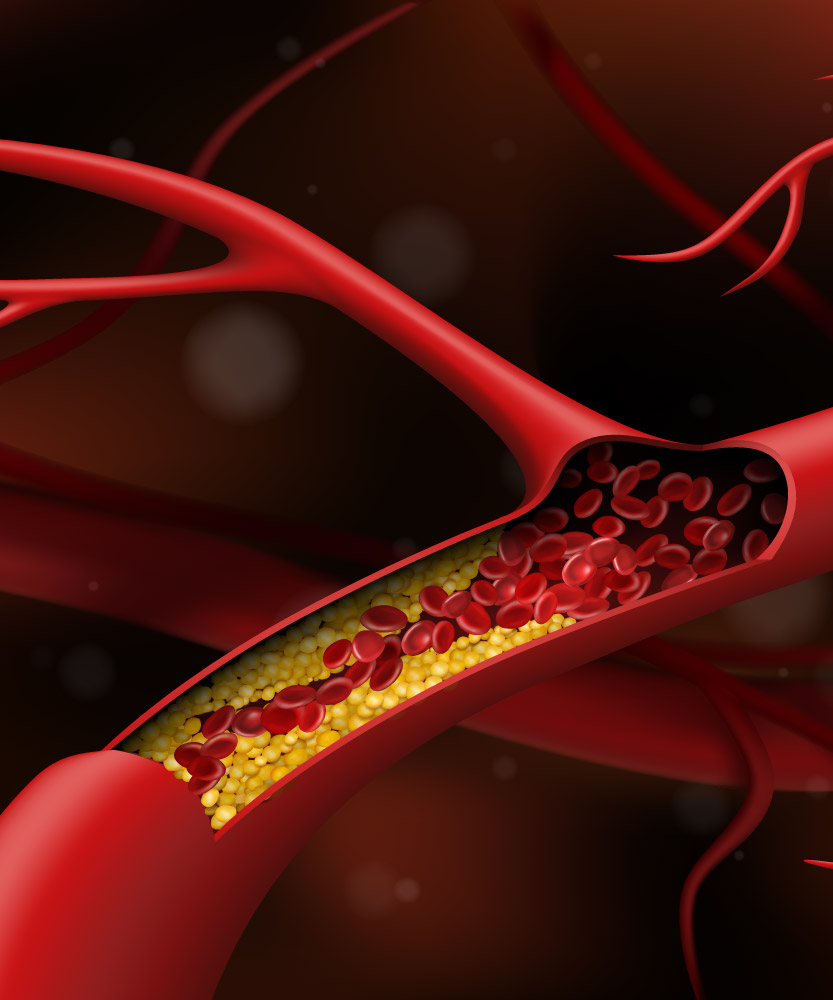
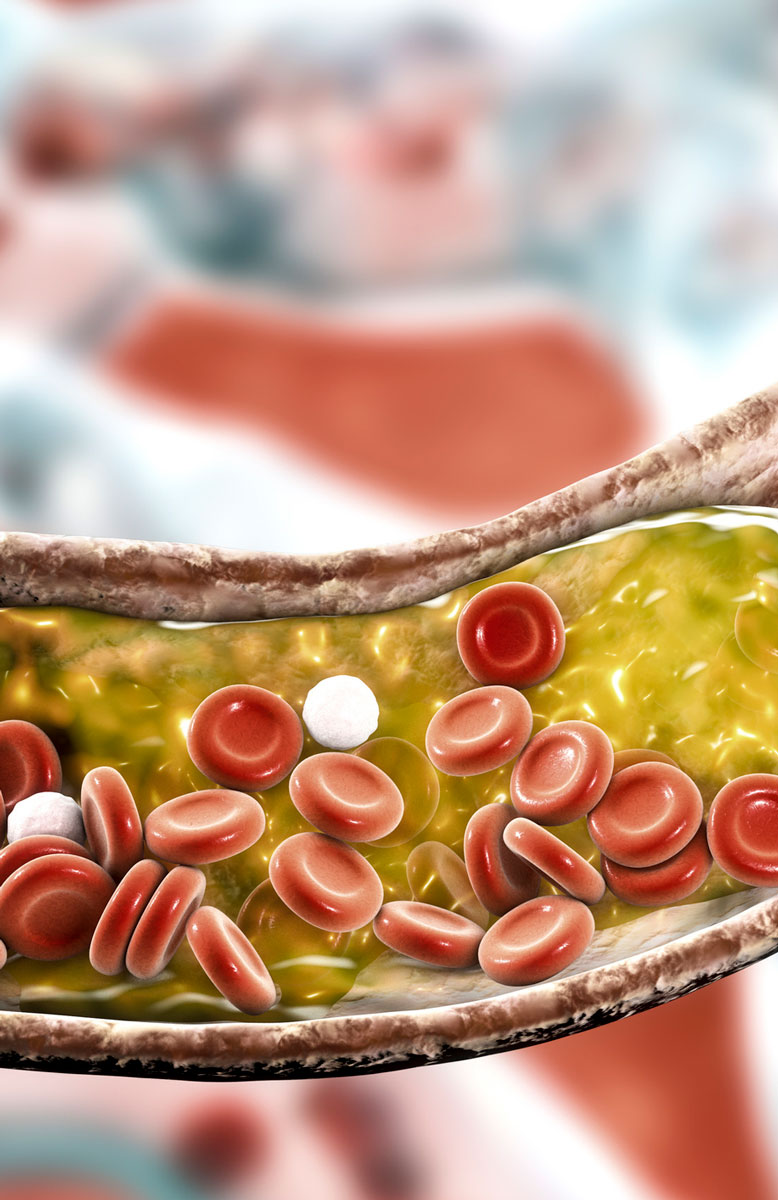
“Good” cholesterol vs “bad” cholesterol
Cholesterol is a fatty substance which is essential to the normal functioning of your body. A certain amount of cholesterol is healthy, however if there is too much cholesterol in the blood, the body is unable to get rid of it and it lodges in the walls of the arteries, forming atheroma (a fatty material or plaque). It is carried throughout the body by molecules called lipoproteins. Over time this fatty build-up of atheroma can narrow the arteries. This process is called Atherosclerosis which can result in a heart attack or stroke.
“Good cholesterol” or high-density lipoprotein cholesterol (HDL-cholesterol) helps remove bad cholesterol from your arteries. A high level of HDL-cholesterol protects against heart disease.
“Bad cholesterol” or low-density lipoprotein cholesterol (LDL-cholesterol) contributes to the build-up of fat deposits in your arteries (atherosclerosis). Over time this build-up leads to a hardening and narrowing of your arteries which can lead to a heart attack or stroke.
Too much bad cholesterol (LDL-cholesterol) is a major driver of ASCVD.
Is it only cholesterol?
In addition to “Good” and “Bad” cholesterol there are two other fatty elements which are linked to ASCVD:
- Triglycerides, which are fats that circulate in the blood stream with cholesterol. High levels of triglycerides are known to increase your risk of ASCVD9.
- Lipoprotein(a), which is structurally very similar to LDL-cholesterol10. Lipoprotein(a) can contribute to plaque buildup and high levels of lipoprotein(a) are mainly due to hereditary reasons11. It is recommended that this should be measured at least once in a person’s lifetime.
- Non-high density lipoprotein cholesterol (non-HDL-C) is another measure of your bad cholesterol and is useful for assessing ASCVD risk in those with high triglyceride levels, diabetes, obesity or very low LDL levels.

Reducing our risks: the right level
Maintaining healthy levels of cholesterol and triglycerides is important for our health. Like blood pressure, a high cholesterol level does not generally cause any symptoms. Your cholesterol level can be measured by taking a simple blood test, which will usually report your overall cholesterol level (total cholesterol); your HDL (good cholesterol); LDL (bad cholesterol); non-HDL-C (bad cholesterol) and triglycerides. It is recommended that adults have their cholesterol checked regularly if they have a cardiac history or are already on cholesterol lowering treatment12.
It is important to acknowledge that some people are not able to achieve the recommended levels of cholesterol through lifestyle changes alone and will require medication if their levels of LDL-cholesterol are too high12. Medication is not a substitute but an add-on to exercise, relaxation, and balanced nutrition. There are different types of treatments that can be prescribed by your doctor to reduce LDL-cholesterol. It is important that your doctor evaluates which is the right medication for you. The adoption of positive lifestyle changes and use of appropriate medical therapies slow down the progression of ASCVD13. This will help lower the risk of cardiac events such as strokes and heart attacks.
- Kronenberg, F. (2021). Lipoprotein(a). In: von Eckardstein, A., Binder, C.J. (eds) Prevention and Treatment of Atherosclerosis. Handbook of Experimental Pharmacology, vol 270. 201-232. Springer, Cham. https://doi.org/10.1007/164_2021_504
- McNeal CJ, Peterson AL. Lipoprotein (a) in Youth. [Updated 2020 Feb 9]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK395570/
- Cybulska B, Kłosiewicz-Latoszek L, Penson PE, Banach M. What do we know about the role of lipoprotein(a) in atherogenesis 57 years after its discovery?. Prog Cardiovasc Dis. 2020;63(3):219-227. doi:10.1016/j.pcad.2020.04.004
- Wilson DP, Jacobson TA, Jones PH, et al. Use of Lipoprotein(a) in clinical practice: A biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol. 2019;13(3):374-392. doi:10.1016/j.jacl.2019.04.010
- Tsimikas S, Fazio S, Ferdinand KC, et al. NHLBI Working Group Recommendations to Reduce Lipoprotein(a)-Mediated Risk of Cardiovascular Disease and Aortic Stenosis. J Am Coll Cardiol. 2018;71(2):177-192. doi:10.1016/j.jacc.2017.11.014
ASCVD through historical lenses
Evidence that our ancient ancestors suffered from ASCVD was revealed in 2009, when a team of researchers performed CT scans on 52 ancient Egyptian mummies. Of the 44 mummies with identifiable cardiovascular tissue, 20 showed probable or definite atherosclerosis, suggesting ASCVD was a widespread affliction even back then.
Learn more here.

Our Mission
Invisible Nation aims to unite a global network of patient organizations and cardiovascular stakeholders to elevate ASCVD as an urgent global health crisis and challenge the status quo.
Invisible Nation will help activate much needed discourse around ASCVD and redefine how stakeholders, including healthcare systems work together to address the world’s leading cause of mortality.
Download a printable infographic on ASCVD:
References:
- Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update from the GBD 2019 Study [published correction appears in J Am Coll Cardiol. 2021 Apr 20;77(15):1958-1959]. J Am Coll Cardiol. 2020;76(25):2982-3021.
- World Health Organization (WHO). Cardiovascular diseases – Data and Statistics. Available at: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases/data-and-statistics. [Last accessed September 2021].
- NIH. National Heart, Lung and Blood Institute – Atherosclerosis. Available at: https://www.nhlbi.nih.gov/health-topics/atherosclerosis#:~:text=Atherosclerosis%20usually%20doesn’t%20cause,and%20symptoms%20of%20the%20disease. [Last accessed September 2021].
- Song P, Fang Z, Wang H, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob Health. 2020;8(5):e721-e729. doi:10.1016/S2214-109X(20)30117-0
- World Health Organization (WHO). Cardiovascular diseases (CVDs). Available at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). [Last accessed August 2021].
- Cholesterol testing and results. MedlinePlus website. Available at https://medlineplus.gov/ency/patientinstructions/000386.htm. [Last accessed September 2021].
- Health screenings for men ages 40 to 64. MedlinePlus website. Available at https://medlineplus.gov/ency/article/007465.htm. [Last accessed September 2021].
- Getting a cholesterol test. Heart UK. Available at https://www.heartuk.org.uk/cholesterol/getting-a-cholesterol-test. [Last accessed September 2021].
- Triglycerides: Why do they matter? Mayo Clinic website. Available at https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/in-depth/triglycerides/art-20048186#:~:text=High%20triglycerides%20may%20contribute%20to,of%20the%20pancreas%20(pancreatitis). [Last accessed September 2021].
- Lipoprotein (a) blood test. MedlinePlus website. Available at https://medlineplus.gov/lab-tests/lipoprotein-a-blood-test/. [Last accessed September 2021]
- Maranhão RC, Carvalho PO, Strunz CC and Pileggi F. Lipoprotein (a): structure, pathophysiology, and clinical implications. Arq Bras Cardiol. 2014 ;103(1) :76-84
- Mach F, Baigent C, Catapano AL, et al. ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111-188
- Lansberg P, Lee A, Lee ZV, Subramaniam K, Setia S. Nonadherence to statins: individualized intervention strategies outside the pill box. Vasc Health Risk Manag. 2018;14:91–102
Thank you for your interest in Invisible Nation. Please complete the optional fields below if you would like to receive updates as new documents and programs are added.






SHARE